We will now explore the various forms of diabetes, their unique characteristics, causes, and management strategies. Understanding the distinctions between these types is crucial for effective diagnosis, treatment, and ongoing care.
Type 1 diabetes, often referred to as insulin-dependent diabetes or juvenile diabetes, is an autoimmune condition in which the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body produces little to no insulin. Type 1 diabetes typically develops during childhood or adolescence, but it can occur at any age.
Causes:
Management:

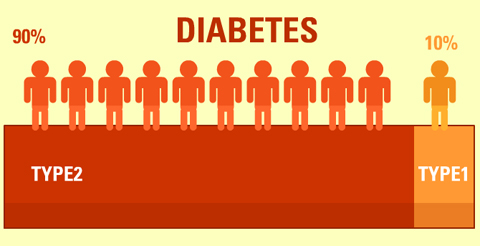
Type 2 diabetes is the most common form of diabetes, characterized by insulin resistance and relative insulin deficiency. In this condition, the body’s cells become resistant to the effects of insulin, and the pancreas may not produce enough insulin to compensate.
Causes:
Management:
Gestational diabetes mellitus (GDM) develops during pregnancy and usually resolves after childbirth. It occurs when the body cannot produce enough insulin to meet the increased demands of pregnancy.
Causes:
Management:
Understanding the different types of diabetes is the first step toward effective management and prevention. If you have any questions or concerns about diabetes types, please consult with a healthcare professional for personalized guidance and support.

200 W. Mines Ave Montebello CA 90640
P.O Box 1347 Montebello, CA 90640 (Mailing Address)
Office: (323) 837-9869
Email: info@lda.org
© 2024 Latino Diabetes Association